which statement is correct regarding glargine insulin?
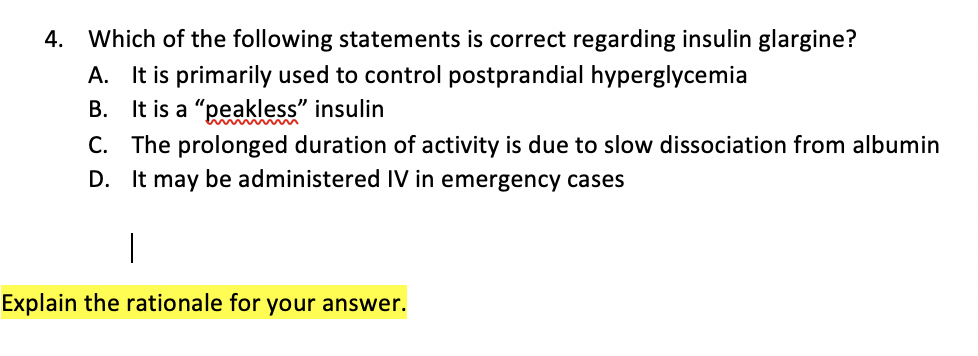 Solved: 4. Which Of The Following Statements Is Correct Re... | Chegg.com
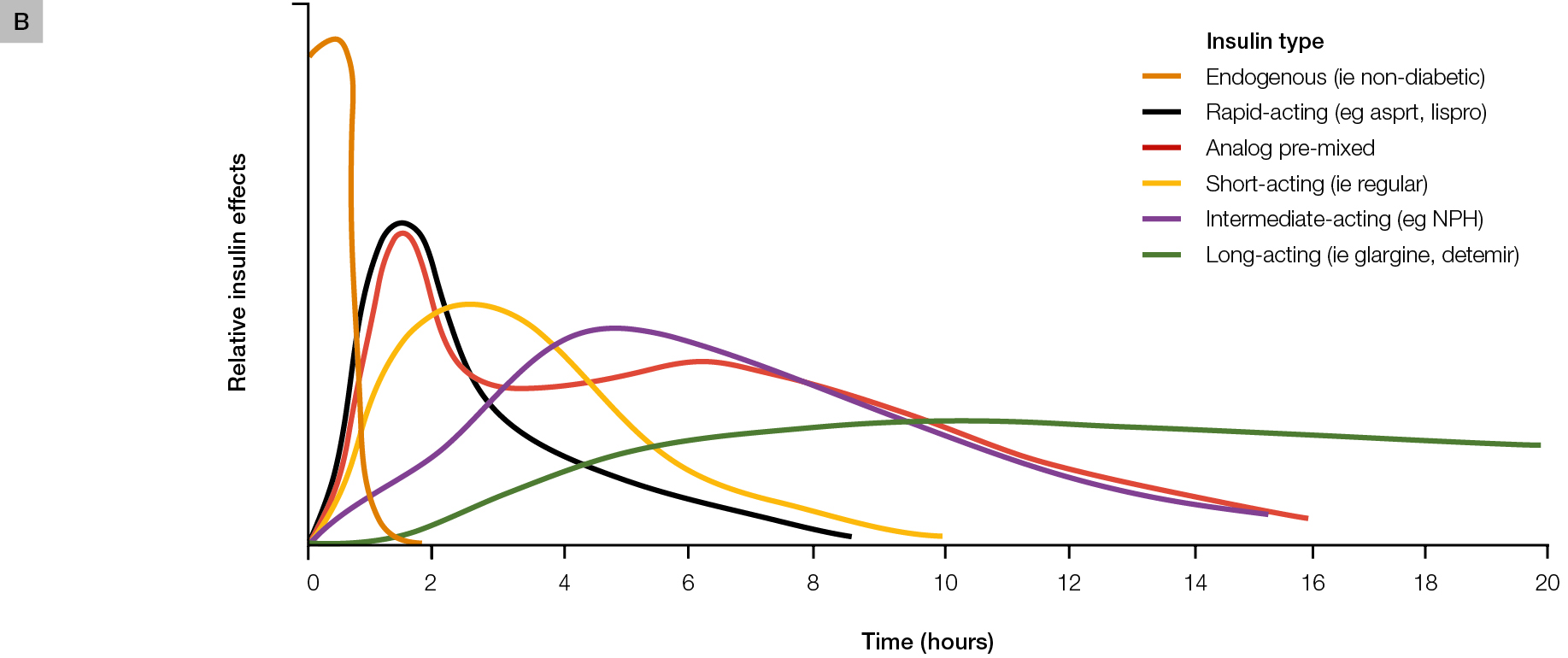
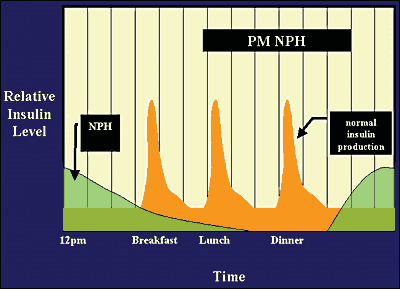
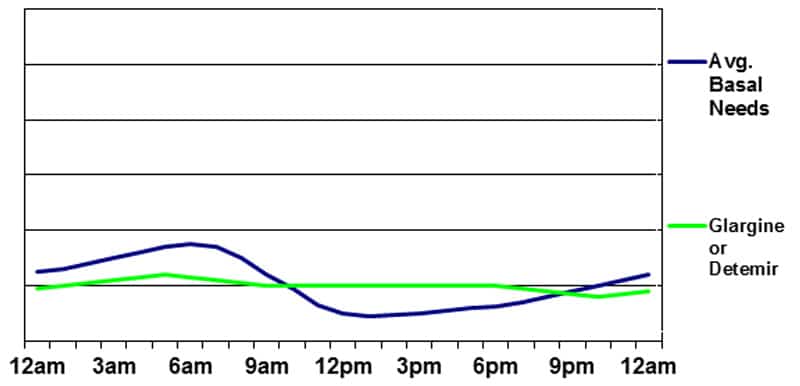
Solved: 4. Which Of The Following Statements Is Correct Re... | Chegg.comAFP IssuesAFP By Topical Collections AFP CME QuizAFP Community BlogSubscribe to AFPInsulin Management of Type 2 Diabetes Mellitus ALLISON PETZNICK, DO, Northern Ohio Medical Specialists, Sandusky, OhioAm Fam Physician. 2011 Jul 15;84(2):183-190. Article SectionInsulin therapy is recommended for patients with type 2 diabetes mellitus and an initial level of A1C over 9%, or if diabetes is uncontrolled despite optimal oral glycemic therapy. Insulin therapy can start as an increase, starting with 0.3 unit per kg or as a replacement, starting with 0.6 to 1.0 unit per kg. By using replacement therapy, 50 percent of the total daily insulin dose is given as basal, and 50 percent as bolus, divided before breakfast, lunch and dinner. Increase therapy may include basal or bolt insulin. Replacement therapy includes basal-bolus insulin and premixed insulin or correction. Glucose control, adverse effects, cost, adherence and quality of life should be considered when choosing therapy. Methformin should continue if possible because it is shown that it reduces mortality from all causes and cardiovascular events in patients with diabetes overweight. In a study comparing premixed insulin, bolt and basal, hypoglyemia was more common with premixed insulin and bolt, and weight gain was more common with the insulin of the bolt. Insulin over time is critical to improving glucemic control and preventing diabetes-related complications. Insulin is continuously secreted by beta cells in a glucose-dependent manner throughout the day. It is also secreted in response to oral carbohydrate loads, including a large first-phase insulin release that suppresses the production of liver glucose followed by a slower second-stage insulin release that covers ingested carbohydrates (). SORT: KEY RECOMMENDATIONS FOR PRACTICE Clinical Recommendation Evidence NoteReferences Similar insulin is as effective as human insulin but is associated with less postprandial hyperglyemia and delayed hypoglycemia. Rapid glucose readings should be used to titrate basal insulin, while preprandial and postprandial glucose readings should be used to titrate the insulin of the food. Lipohipertrophy due to repeated injections of insulin in the same area leads to poor insulin absorption and can cause early postprandial hyperglycemia and/or delayed hypoglycemia. CMetformin (Glucophage) combined with insulin is associated with a lower weight gain, a lower dose of insulin and less hypoglycemia compared to insulin alone. BOral medications should not be abruptly suspended when initiating insulin therapy due to the risk of rebounding hyperglycemia. CAnalogo insulin is as effective as human insulin but is associated with less postprandial hyperglyemia and delayed hypoglycemia. Rapid glucose readings should be used to titrate basal insulin, while preprandial and postprandial glucose readings should be used to titrate the insulin of the food. Lipohipertrophy due to repeated injections of insulin in the same area leads to poor insulin absorption and can cause early postprandial hyperglycemia and/or delayed hypoglycemia. CMetformin (Glucophage) combined with insulin is associated with a lower weight gain, a lower dose of insulin and less hypoglycemia compared to insulin alone. BOral medications should not be abruptly suspended when initiating insulin therapy due to the risk of rebounding hyperglycemia. CA = consistent and good quality patient-oriented tests; B = incoherent or limited quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion or case series. For information on the SORT test rating system, go to . SORT: KEY RECOMMENDATIONS FOR PRACTICE Clinical Recommendation Evidence NoteReferences Similar insulin is as effective as human insulin but is associated with less postprandial hyperglyemia and delayed hypoglycemia. Rapid glucose readings should be used to titrate basal insulin, while preprandial and postprandial glucose readings should be used to titrate the insulin of the food. Lipohipertrophy due to repeated injections of insulin in the same area leads to poor insulin absorption and can cause early postprandial hyperglycemia and/or delayed hypoglycemia. CMetformin (Glucophage) combined with insulin is associated with a lower weight gain, a lower dose of insulin and less hypoglycemia compared to insulin alone. BOral medications should not be abruptly suspended when initiating insulin therapy due to the risk of rebounding hyperglycemia. CAnalogo insulin is as effective as human insulin but is associated with less postprandial hyperglyemia and delayed hypoglycemia. Rapid glucose readings should be used to titrate basal insulin, while preprandial and postprandial glucose readings should be used to titrate the insulin of the food. Lipohipertrophy due to repeated injections of insulin in the same area leads to poor insulin absorption and can cause early postprandial hyperglycemia and/or delayed hypoglycemia. CMetformin (Glucophage) combined with insulin is associated with a lower weight gain, a lower dose of insulin and less hypoglycemia compared to insulin alone. BOral medications should not be abruptly suspended when initiating insulin therapy due to the risk of rebounding hyperglycemia. CA = consistent and good quality patient-oriented tests; B = incoherent or limited quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert opinion or case series. For information on the SORT test rating system, go to . Figure 1.Figure 1.Insulin is secreted by the pancreas continuously throughout the day, as well as in response to oral carbohydrate loads. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010. Figure 1.Insulin is secreted by the pancreas in a way dependent on glucose continuously throughout the day, as well as in response to oral carbohydrate loads. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010. Type 2 diabetes mellitus is associated with insulin resistance and progressively progressive beta cell failure. Over time, type 2 diabetes is diagnosed in patients, up to half of their beta cells do not work properly. The failure of beta cells continues at a rate of about 4% each year. Thus, patients with type 2 diabetes often benefit from insulin therapy at some point after diagnosis. Concerns about Insulin Therapy Pain, weight gain, and hypoglycemia may occur with insulin therapy. Pain is associated with glucose injection and monitoring therapy, although there are now thinner and shorter needles available to help decrease pain. The weight gain associated with insulin therapy is due to the anabolic effects of insulin, increased appetite, defensive feeding of hypoglycemia and increased caloric retention associated with decreased glucosuria. In the UK. Study of Prospective Diabetes, patients with type 2 diabetes who were taking insulin obtained an average of 8 pounds, 13 oz (4 kg), which was associated with a decrease of 0.9% in level A1C compared to patients in conventional therapy. Hypoglycemia may occur from a misalignment between insulin and carbohydrate intake, exercise or alcohol use. Hypoglycemia has been associated with increased risk of dementia and may have implications for heart arrhythmia. , All patients should be instructed on symptoms and treatment of hypoglycemia. The guidelines of the American Diabetes Association (ADA) recommend that the blood glucose level be checked if hypoglycemia is suspected (glucose level less than 70 mg per dL [3.89 mmol per L]), then treated with a fast-acting carbohydrate, such as juice or glucose tablets. The blood glucose level should be checked after 15 minutes to ensure that it has been standardized. An epidemiological study has raised concerns about the risk of glargine (Lantus) and other insulin therapies. Glagine is theoretically more likely to cause cancer due to its high affinity for insulin-like growth factor receptor. A consensus statement by ADA indicates that this potential risk needs further research, but it should not be a limiting factor in the choice of treatment. Finally, it is important to note that randomized controlled trials have not been conducted to demonstrate a reduction in full-cause mortality or cardiovascular events with increased insulin in patients with type 2 diabetes. Initiating appropriate insulin therapy American College of Endocrinology and the American Association of Clinical Endocrinologists recommend the initiation of insulin therapy in patients with type 2 diabetes and an initial level of A1C over 9 percent, or if diabetes is unchecked despite optimal oral glycemic therapy. Insulin can be used alone or in combination with oral medications, such as metformin (Glucophage). This recommendation is based on expert opinion, and not on randomized controlled test results that compare different approaches in patients with an initial level of A1C over 9%. In the UK. Study of Prospective Diabetes, early intensive glucose control starting with sulfonylurea, then metformin, then insulin was associated with a 25% reduction in microvascular complications and a risk reduction of 12 percent at any final point related to diabetes, but it was not associated with a reduction in mortality for all causes. A subgroup of patients randomized to intensive therapy with metformin alone had a 36 percent reduction in mortality for all causes. This is consistent with current ADA guidelines that recommend using metformin as frontline pharmacological therapy; however, additional therapies should be added if diabetes is not controlled only with metformin. Recent trials have shown that intensive glucose control (i.e., an A1C target of less than 6.0 or 6.5%) does not improve, and can worsen, clinical results. – Older patients with limited life expectancy and patients with high risk of hypoglycemia, previous cardiovascular disease, or advanced microvascular disease, longer diabetes duration or multiple comorbid conditions may benefit from less strict glucose control. Analogue Versus Human InsulinGlucose control, adverse effects, cost, adherence and quality of life should be considered when choosing a type of insulin. In general, analog insulin is similar to human insulin in diabetes control, although some trials have found higher average levels in patients taking analog insulin compared to human insulin. Analog insulin usually causes less postprandial hyperglycemia and delayed hypoglycemia. In a recent meta-analysis, glucemic control was not improved with analogue insulin compared to human insulin, but night hypoglycemia was reduced. An industry-funded cost-effectiveness analysis found that the increasing cost of medication is more than extinguished by the reduction of hypoglycemic events. However, the analysis assumed a 14 percent cost differential, which is inconsistent with current prices ($119 for a 10 ml insulin bottle compared to $73 for a 10 ml insulin bottle [Humulin N], a 63 percent difference. , Cost-effectiveness analysis has differed in relation to long-term savings in the use of analogue insulin in patients with type 2 diabetes, with industry-sponsored studies that find lower costs and government-sponsored studies that find no cost reduction. Adherence and quality of life with analog insulin have been improved compared to human insulin. ,Choose the right type of insulinInsulin regimens must adapt to the patient's needs and lifestyle. One of the most important considerations is pharmacokinetics of different insulin preparations (and ). defines commonly used terms in insulin therapy. 30 minutes to 30 hours 30 minutes to 30 hours . Access 6 December 2010. Figure 2.Figure 2.Initiation of action, peak and duration of exogenous preparations for insulin. Adapted from Hirsch IB. Insulin analogs. N Engl J Med. 2005;352(2):177. Figure 2.Starting of action, peak and duration of preparations for exogenous insulin. Adapted from Hirsch IB. Insulin analogs. N Engl J Med. 2005;352(2):177. Common Terms of Use in Insulin TherapyTermDefinitionCalculationAugmentation Using basal or bolt insulin to help improve glucose control in patients with partial beta-cellular insufficiency0. 3 unit per kg Use of basal insulin and the ball to control glucose in the blood when the production of endogenous insulin is minimal or absent0.6 to 1.0 unit per kg The number of insulin units needs to cover for a certain number of ingested carbohydrates500 divided by total insulin (usually about 1 unit per 10 g) Correction (sensitivity) 3 unit per kg Use of basal insulin and bolo to control glucose in the blood when the production of endogenous insulin is minimal or absent0.6 to 1.0 unit per kg The number of insulin units needs to cover for a certain number of ingestible carbohydrates 500 divided by total insulin (normally about 1 unit per 10 g) Use of basal or bolt insulin to help improve glucose control in patients with partial beta-cellular insufficiency0. 3 unit per kg Use of basal insulin and the ball to control glucose in the blood when the production of endogenous insulin is minimal or absent0.6 to 1.0 unit per kg The number of insulin units needs to cover for a certain number of ingested carbohydrates500 divided by total insulin (usually about 1 unit per 10 g) Correction (sensitivity) 3 unit per kg Use of basal insulin and bolo to control glucose in the blood when the production of endogenous insulin is minimal or absent0.6 to 1.0 unit per kg The number of insulin units required to cover a certain number of ingested carbohydrates 500 divided by total daily insulin (usually about 1 unit per 10 g) Correction (sensitivity) The levels of A1C were similar among the groups, but hypoglycemia was more common in the premixing and bolt groups, and weight gain was more common in the group of bolts. The results of this study suggest that adding basal insulin to oral antihyperglycemia is equally effective but has less adverse effects compared to adding premixed insulin or bolt The goal of basal insulin is to suppress the production of liver glucose and improve fasting hyperglyemia (). If basal insulin is too high, it will also partially cover meals and lead to hypoglycemia during the night or if a meal is lost. Analog insulin of prolonged action can be given once or twice a day, depending on the dose. Lower doses may not last 24 hours, while higher doses may prevent insulin absorption. NPH can be administered from one to three times a day. HNP is often used during pregnancy and in patients who cannot afford the initial cost of analogue insulin. Figure 3.Figure 3.Based insulin magnification therapy. Pharmacokinetic profile of using glargine, detemir or NPH therapy once a day. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010. Chart 3.Figure 3.Based insulin magnification therapy. Pharmacokinetic profile of using glargine, detemir or NPH therapy once a day. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010. Insulin Bolus can also be used to increase ( ). Short-acting insulin is given before meals to cover the carbohydrate load. Analog short-acting insulin is given up to 15 minutes before a meal to maintain the two-hour postprandial glucose levels. Taking insulin after meals increases the risk of early postprandial hyperglyemia followed by delayed hypoglycemia. Regular insulin can be used instead and is given 30 to 45 minutes before meals. Figure 4.Figure 4.Based insulin replacement therapy. Pharmacokinetic profile of using glargine once a day, detemir twice a day, or NPH twice a day along with an analog short action insulin before each meal. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010. Figure 4.Figure 4.Basal-bolus insulin replacement therapy. Pharmacokinetic profile of using glargine once a day, detemir twice a day, or NPH twice a day along with an analog short action insulin before each meal. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed December 10, 2010.REPLACEMENTThe replacement therapy includes basal-bolus insulin and premixed insulin or correction; an insulin pump may be used, but it is beyond the scope of this article. Replacement should be considered for patients with type 2 diabetes who are not controlled by increased therapy and who are able to comply with such a regime or who want stricter control. Insulin Bolus should be added to basal insulin if fasting glucose goals are met, but postprandial targets are not met. When blood glucose levels are above predefined targets, additional short-acting insulin can be added to the bolt dose before meals. For example, a patient takes 40 units of daily glargine and 12 units of lispro (Humalog) before each meal, and has a correction factor of 1 unit per 20 mg per dL (1.11 mmol per L) above 120 mg per dL (6.66 mmol per L). If the blood glucose level in the breakfast is 160 mg per dL (8.88 mmol per L), the patient would take 12 lispro units for the meal plus 2 additional units for the correction before eating. Premixed insulin similarly reduces A1C compared to basal-bolus insulin. NPH is combined with regular insulin or short-acting analog insulin and is administered twice or three times a day. Less injections are necessary, but patients are more restricted in their eating habits and schedules. Patients should eat breakfast, lunch, dinner and possibly half a morning and snacks to prevent hypoglycemia. If used, the insulin correction should be given separately with a short-acting insulin. This can increase the number of injections compared to basal-bolus therapy (). Figure 5.Figure 5.Merged insulin therapy. Pharmacokinetic profile of using a regular short-acting analog insulin or insulin along with NPH in a premixed insulin regimen. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010. Figure 5Figure 5.Merged insulin therapy. Pharmacokinetic profile of using a regular short-acting analog insulin or insulin along with NPH in a premixed insulin regimen. Adapted with permission from Diabetes Education Online. University of California, San Francisco. Access December 10, 2010.Initiation, Titting and TrackingThe initial dose of insulin is individualized according to the patient's insulin sensitivity. Insulin therapy can start with a dose of ensemble, such as 10 units of daily glargine, or by using weight-based equations. In the list of categories for estimating increase, replacement, carbohydrate ratio and correction therapy. By using replacement therapy, 50 percent of the total daily insulin dose is given as basal and 50 percent as bolus, divided before breakfast, lunch and dinner. For example, a 120 kg (265 lb) patient requiring basal insulin and correction would need 36 basal insulin units (0.3 unit per kg); 12 short-acting insulin units before each meal (0.3 unit per kg divided between three meals); and, for correction, 1 unit of a short-acting insulin for every 25 mg per duco (1.39 mmol per L) fixed. Insulin over time is critical to improving glucemic control and preventing diabetes-related complications. , ADA's current targets for glucose control are described in . Fasting glucose readings are used for titrate-based insulin, while preprandial and postprandial glucose readings are used for food insulin. Doctors can increase or decrease basal insulin and/or bolts by 10 percent based on glucose readings in the patient's home. Some doctors have adopted the Treat-to-Target test titration schedule for basal insulin (). It is also safe and effective to give patients autonomy to adjust insulin on their own. Typically, insulin is increased or decreased by 2 to 3 units every three to seven days if the blood glucose level of the patient is not within the targets set. American Diabetes Association Blood Glucose and A1C Goals for Patients with Diabetes MellitusMeasurementGeneral population Pregnant glucose in fasting blood90 to 130 mg per dL (5 to 7.21 mmol per L)60 to 100 mg per dL (3.33 to 5.55 mmol per L) glucose 100Gucosa in fasting blood90 to 130 mg per dL (5 to 7.21 mmol Some microvascular benefits have been associated with A1C targets of 6.0 or 6.5%. Adapted with permission from American Diabetes Association. Health Care Standards in Diabetes—2010 [The corrigendum published appears in Diabetes Care. 2010;33(3):692]. Care for diabetes. 2010033(suppl 1):S11–S61.American Diabetes Association Blood Glucose and A1C Goals for Patients with Diabetes MellitusMeasurementGeneral population Pregnant women glucose in fasting blood90 to 130 mg per dL (5 to 7.21 mmol per L)60 to 100 mg per dL (3.33 to 5.55 mmol per L) Some microvascular benefits have been associated with A1C targets of 6.0 or 6.5%. Adapted with permission from American Diabetes Association. Health Care Standards in Diabetes—2010 [The corrigendum published appears in Diabetes Care. 2010;33(3):692]. Care for diabetes. 2010;33(suppl 1):S11–S61. Illustration by L1 x1.9 per cent The Treat-to-Target trial: randomized addition of glargine or human insulin of HNP to oral therapy of type 2 diabetic patients. Care for diabetes. 2003;26(11):3081. L1 per L1 x L1 x L1 =============================================================================================================================================================================================================================================== The Treat-to-Target trial: randomized addition of glargine or human insulin of HNP to oral therapy of type 2 diabetic patients. Care for diabetes. 2003;26(11):3081. Patients should go to the doctor's office for follow-up at least every three to four months. The communication frequency of insulin titration through clinical contact, telephone, e-mail or fax is highly correlated with the improvement of A1C levels. , Insulin Insulin Insulin is only effective if properly administered. Injections can be given in the abdomen, outer thigh, back of the arm, and the region of flanks and buttocks. The needle should be placed at an angle of 90 degrees to the skin and kept in place for five to 10 seconds after the injection to prevent insulin leak. The rotation of injection sites is important to prevent lipohipertrophy (i.e., the scar tissue of repeated injections in the same area). Lipohipertrophy leads to poor insulin absorption and deposit formation, which can randomly release insulin, causing early postprandial hyperglyemia and/or delayed hypoglyemia. Insulin is available in pens and vials. The benefits of insulin pens include the comfort of storing at room temperature for 28 days after opening and ease of use for patients with visual problems or skill. Patients with visual difficulties can listen to the "clicks" of the insulin pen to count the number of units. Patients should be instructed to prepare the insulin pen before each use. Priming consists of the preparation of 1 or 2 units of insulin and injection in the air to allow insulin to fill the needle. Using Insulin with Oral Medicines Many oral medications are safe and effective when combined with insulin therapy. To maximize profit without causing significant adverse effects, it is important to consider the mechanism of action for different therapies. Insulin sensitizers have been proven safe and effective when combined with insulin therapy. , Methformine is usually continued indefinitely after the patient begins insulin therapy because it reduces cardiovascular risk in patients with overweight type 2 diabetes. Methformin combined with insulin is also associated with a weight reduction, a lower insulin dose and less hypoglyemia compared to insulin alone. Tiazolidines improve insulin sensitivity but can increase weight gain, fluid retention and the risk of congestive heart failure when combined with insulin. Tiazolidinediones have also failed to demonstrate a reduction in macrovascular complications or mortality from all causes. Alphaglycosidase inhibitors delay carbohydrate absorption in the gastrointestinal tract to decrease postprandial hyperglycemia. These medicines are safe and effective when combined with insulin. Insulin secretgogues (sulfonylureas and glytinides) can be combined with insulin, especially when only the basal increase is used. However, there is a possible increase in the risk of hypoglyemia that should be monitored closely. Usually, for when insulin is needed for meals, secret insulin is not effective or necessary. However, it is recommended to continue oral medications while insulin is started to prevent rebound hyperglyemia. After diabetes is controlled, the patient can get rid of oral medications. Incredulin therapies include dipeptidyl-peptidase IV inhibitors (sitagliptin [Januvia] and saxagliptin [Onglyza]) and peptide agonists-1 (exenatide [Byetta] and liraglutide [Victoza]). Sitagliptin is currently the only one of these medications that is approved by the U.S. Food and Drug Administration for insulin- combined therapy. This combination is associated with improved fasting and postprandial glucose control. Exenatide combined with insulin has been associated with better glucemic control, weight loss and no higher risk of hyperglycemia. As with thiazolidinediones, peptides-1 agonists and glucagon saxagliptin have not been shown to reduce macrovascular events or mortality for all causes. Data Sources: A PubMed search was completed in clinical consultations using the key terms in intensive insulin, insulin and cancer, insulin and weight gain, UKPDS, insulin autotitration, human and analog insulin, metformin and insulin, sulfonilurea and insulin, and increlin and increlin. The search included meta-analysis, randomized controlled trials, clinical trials and revisions. Search dates: August 24, 2010 and November 29, 2010. Read the full article. Read the full article. Already a member/subscriber? Purchase Access: Already a member or subscriber? Best Value! Get full access from $140 Access This Issue$39.95 Access This Article$20.95 $(."ui-dialog.ui-widget.ui-widget-content.ui-corner-all.subscriptionmodal.ui-draggable").addClass("dept"); Already a member or subscriber? The best value! Get full access This problem Access to this article $(."ui-dialog.ui-widget.ui-widget-content.ui-corner-all.subscriptionmodal.ui-draggable").addClass("dept"); The AuthorALLISON PETZNICK, DO, is a family doctor at Firelands Regional Medical Centers in Sandusky, Ohio. He is also a family doctor and diabetologist with medical specialists from northern Ohio in Sandusky....Add correspondence with Allison Petznick, DO, medical specialists from northern Ohio, 1200 W. Strub Rd., Ste. 230, Sandusky, OH 44870 (e-mail: ). The author has no reprints. Author's information: There are no relevant financial affiliations to disclose. REFERENCES1. Ritzel RA, Bulter PC. Physiology of glucose homeostasis and insulin secretion. In: Leahy JL, Cefalu WT, eds. Insulin therapy. New York, NY: Marcel Dekker; 2002:61–72....2. Diabetes Education Online. University of California, San Francisco. Accessed 10 December 2010.3. Gastaldelli A, Ferrannini E, Miyazaki Yes. Matsuda M, DeFronzo RA. Betacellular dysfunction and glucose intolerance: results of the study of the metabolism of San Antonio (SAM). Diabetology. 2004;47(1):31–39.4. U.K. Prospective Diabetes Study 16. Summaries of type II diabetes 6-year therapy: progressive disease. U.K. Prospective Diabetes Study (UKPDS) Group [published correction appears in Diabetes 1996;45(11): 1655]. Diabetes. 1995;44(11):1249-1258.5. Intensive glucose control with sulfonylures or insulin compared to conventional treatment and the risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–853.6. Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP Jr, Selby JV. hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA. 2009;301(15):1565–1572.7. Lindström T, Jorfeldt L, Tegler L, Arnqvist HJ. Hypoglycemia and heart arrhythmias in patients with type 2 diabetes mellitus. Diabet Med. 1992;9(6):536-541.8. American Diabetes Association. Insulin administration. Watch your diabetes. 2004;27(suppl 1):S106–S109.9. Jonasson JM, Ljung R, Talbäck M, Haglund B, Gudbjörnsdòttir S, Steineck G. The use of insulin glargine and the short-term incidence of malignities, a population-based follow-up study in Sweden. Diabetology. 2009;52(9):1745-1754.10. Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and Cancer: a consensus report. Watch your diabetes. 2010;33(7):1674-1685.11. Jellinger PS, Davidson JA, Blonde L, et al. Route maps to achieve glucemic control in type 2 diabetes mellitus: ACE/AACE Diabetes Road Map Task Force. Endocr Pract. 2007;13(3):260-268.12. UK Effect of intensive glucose control with metformin on complications in patients with overweight with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group [published correction appears in Lancet. 1998;352(9139):1558]. Lancet. 1998;352(9131):854–865.13. Gerstein HC, Miller ME, Byington RP, et al. ; Action to Cardiovascular Control Risk in Diabetes Study Group. Effects of the intensive decrease in glucose in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559.14. Patel A, MacMahon S, Chalmers J, et al. ; ADVANCE Collaborative Group. Intensive blood glucose control and vascular results in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–2572.15. Duckworth W, Abraira C, Moritz T, et al. ; VADT researchers. Glucose control and vascular complications in veterans with type 2 diabetes [Public corrections appear in N Engl J Med. 2009;361(10):1028 and N Engl J Med. 2009;361(10):1024-1025]. N Engl J Med. 2009;360(2):129-139.16. American Diabetes Association. Health Care Standards in Diabetes—2010 [The corrigendum published appears in Diabetes Care. 2010;33(3):692]. Watch your diabetes. 2010;33(suppl 1):S11–S61.17. Singh SR, Ahmad F, Lal A, Yu C, Bai Z, Bennett H. Effectiveness and safety of insulin analogues for managing diabetes mellitus: a metaanalysis. CMAJ. 2009;180(4):385–397.18. Ross SA, Zinman B, Fields RV, Strack T; Canadian Lispro Study Group. Comparative study of insulin lispro and regular human insulin in patients with type 2 diabetes mellitus and secondary insufficiency of oral hypoglycemic agents. Clin Invest Med. 2001;24(6):292–298.19. Tolerance and Glucose Mortality: comparison of diagnostic criteria of WHO and the American Diabetes Association. The study group DECODE. European Diabetes Epidemiology Group. Epidemiology of diabetes: collaborative analysis of diagnostic criteria in Europe. Lancet. 1999;354(9179):617-621.20. Bullano MF, Al-Zakwani IS, Fisher MD, Menditto L, Willey VJ. Differences in hypoglycemia events rates and associated cost-cost ratio in patients initiated in long- and intermediate-acting insulin products. Curr Med Res Opin. 2005;21(2):291–298.21. Drugstore.com. Accessed January 9, 2011.22. Brändle M, Azoulay M, Greiner RA. Cost effectiveness and insulin-erotility glargine compared to NPH insulin based on a 10-year long-term complications simulation with the Diabetes Mellitus Model in patients with type 2 diabetes in Switzerland. Int J Clin Pharmacol Ther. 2007;45(4):203–220.23. Cameron CG, Bennett HA. Cost effectiveness of insulin analogs for diabetes mellitus. CMAJ. 2009;180(4):400–407.24. Howorka K, Pumprla J, Schlusche C, Wagner-Nosiska D, Schabmann A, Bradley C. Treat with the level of satisfaction of roof-based treatment in patients with diabetes under flexible and functional insulin treatment. Qual Life Res. 2000;9(8):915–930.25. Fritsche A, Schweitzer MA; Häring HU; 4001 Study Group. Glimepiride combined with morning insulin glargine, neutral protamine insulin in bedtime or insulin glargine in patients with type 2 diabetes. A randomized and controlled trial. Ann Intern Med. 2003;138(12):952–959.26. Endotext.org. Management of type I diabetes. . Access December 6, 2010.27. Hirsch IB. Insulin analogs. N Engl J Med. 2005;352(2):174–183.28. Holman RR, Farmer AJ, Davies MJ, et al. ; Study Group 4-T. Triennial performance of complex insulin regimens in type 2 diabetes [the published correction appears in N Engl J Med. 2010; 363(21): 2078]. N Engl J Med. 2009;361(18):1736-1747.29. Cobry E, McFann K, Messer L, et al. The time of insulin screws to achieve optimal postprandial glycosmic control in patients with type 1 diabetes. Tecnol de Diabetes. 2010;12(3):173-177.30. Miser WF, Arakaki R, Jiang H, Scism-Bacon J, Anderson PW, Fahrbach JL. Random, open, side-by-side evaluations of basal-bolus therapy versus premixed insulin lispro therapy in patients with type 2 diabetes mellitus do not manage with initial insulin treatment and continuous oral antihyperglycemic drugs: a substudy of intensification of the non-lower DURABLE trial. Clin Ther. 2010;32(5):896–908.31. Riddle MC, Rosenstock J, Gerich J; Insulina Glargine 4002 Researchers. The Treat-to-Target trial: randomized addition of glargine or human insulin of HNP to oral therapy of type 2 diabetic patients. Watch your diabetes. 2003;26(11):3080–3086.32. Ligthelm RJ. Aspart 30/70 biophase insulin autotitration improves glucaemic control and allows easy intensification in a Dutch clinical practice. Primary care diabetes. 2009;3(2):97-102.33. Kennedy L, Herman WH, Strange P, Harris A; GOAL A1C Team. Impact of the active versus usual algorithmic titration of basal insulin and measurement of the care point compared to the measurement of HbA1c laboratory in the glucemic control in patients with type 2 diabetes: glucemic optimization with algorithms and laboratories in the Point of Care study (GOAL A1C). Watch your diabetes. 2006;29(1):1-8.34. Swinnen SG, Devries JH. The contact rate determines the result of insulin initiation trials based on type 2 diabetes. Diabetology. 2009;52(11):2324–2327.35. Johansson UB, Amsberg S, Hannerz L, et al. Deficient absorption of insulin asparts from lipohypertrophic injection sites. Watch your diabetes. 2005;28(8):2025–2027.36. Berhanu P, Perez A, Yu S. Effect of pioglitazone in combination with insulin therapy in glucaemic control, insulin dose requirement and lipid profile in patients with type 2 diabetes previously poorly controlled with combined therapy. Metab obese diabetes. 2007;9(4):512–520.37. Avilés-Santa L, Sinding J, Raskin P. Methformin effects in patients with poorly controlled diabetes mellitus and insulin-treated. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1999;131(3):182–188.38. Stratton IM, Adler AI, Neil HA, et al. Glycemia association with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412.39. Kelley DE, Bidot P, Freedman Z, et al. Effectiveness and safety of acarbosa in patients treated with type 2 diabetes. Watch your diabetes. 1998;21(12):2056–2061.40. Riddle MC, Schneider J. Start the insulin treatment of obese patients with night insulin 70/30 plus glimepiride versus insulin alone. Glimepiride Combination Group. Watch your diabetes. 1998;21(7):1052–1057.41. Vilsbøll T, Rosenstock J, Yki-Järvinen H, et al. Effectiveness and safety of sitagliptin when added to insulin therapy in patients with type 2 diabetes. Metab obese diabetes. 2010;12(2):167-177.42. Sheffield CA, Kane MP, Busch RS, Bakst G, Abelseth JM, Hamilton RA. Safety and efficacy of exenatide in combination with insulin in patients with type 2 diabetes mellitus. Endocr Pract. 2008;14(3):285–292. Copyright © 2011 by the American Academy of Family Physicians. This content is owned by AAFP. A person who sees it online can make an impression of the material and can use that impression only for his personal and non-commercial reference. This material cannot be downloaded, copied, printed, stored, transmitted or reproduced in any medium, either now known or later invented, except as authorized in writing by AAFP. Contact for copyright questions and/or permission requests. You want to use this article somewhere else? More in AFPEditor's collectionsLearn more in PubmedMOST RECENT ISSUEMar 1, 2021Mar 1, 2021Access to the latest issue of American Family PhysicianEmail Alerts Don't miss a single problem. Subscribe to the AFP free content table. Browse this articleContinue reading Previous: Previous: Next: / / / / Insulin management of type 2 diabetes Mellitus Copyright © 2020 American Academy of Family Physicians. All rights reserved.
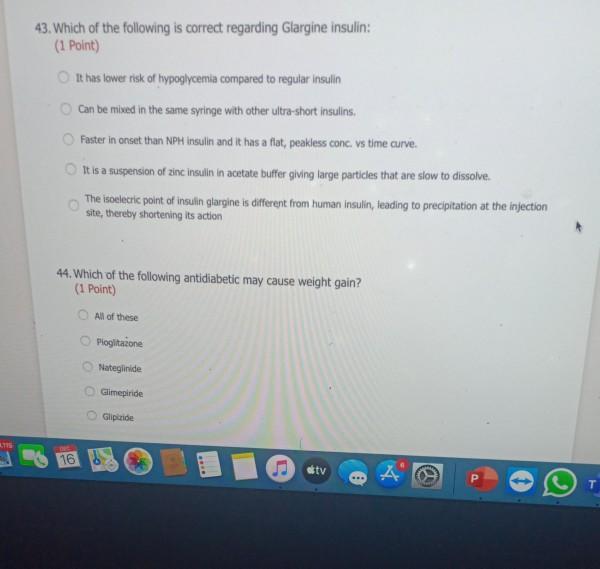
Solved: 43. Which Of The Following Is Correct Regarding Gl... | Chegg.com
Solved: 43. Which Of The Following Is Correct Regarding Gl... | Chegg.com
Solved: 43. Which Of The Following Is Correct Regarding Gl... | Chegg.com
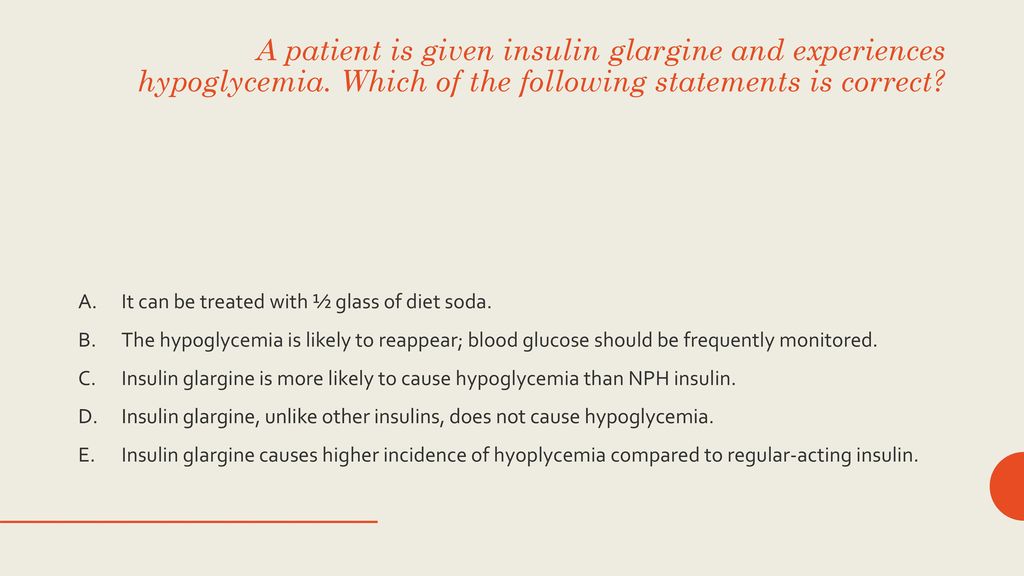
Diabetes Tutoring By Alaina Darby. - ppt download

Diabetes Treatment Options | Lantus® (insulin glargine injection) 100 Units/mL

Learn How to Inject Lantus | Lantus® (insulin glargine injection) 100 Units/mL

Learn How to Inject Lantus | Lantus® (insulin glargine injection) 100 Units/mL
Insulin Analogs :: Diabetes Education Online

Types of Insulin Chart: Duration, Comparison, and More

Toujeo vs Lantus® | Toujeo® (insulin glargine injection) 300 Units/mL
RACGP - The introduction of insulin in type 2 diabetes mellitus
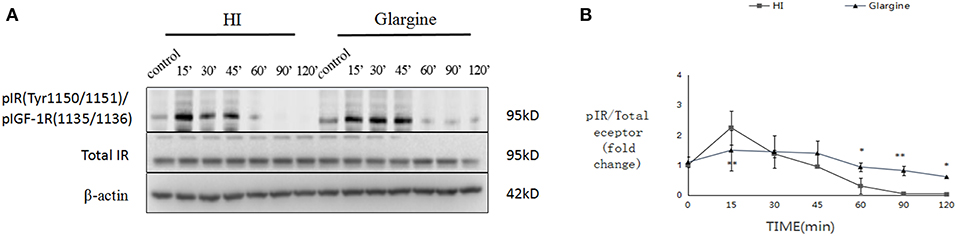
Frontiers | The Role of Insulin Glargine and Human Insulin in the Regulation of Thyroid Proliferation Through Mitogenic Signaling | Endocrinology
![Lantus (Insulin Glargine [rDNA origin] Injection): Uses, Dosage, Side Effects, Interactions, Warning Lantus (Insulin Glargine [rDNA origin] Injection): Uses, Dosage, Side Effects, Interactions, Warning](https://images.rxlist.com/images/rxlist/lantus2.gif)
Lantus (Insulin Glargine [rDNA origin] Injection): Uses, Dosage, Side Effects, Interactions, Warning

Insulin – Pharmacology, Therapeutic Regimens, and Principles of Intensive Insulin Therapy - Endotext - NCBI Bookshelf

Improved Glycemic Control vs NPH | Lantus® (insulin glargine injection) 100 Units/mL

Insulin – Pharmacology, Therapeutic Regimens, and Principles of Intensive Insulin Therapy - Endotext - NCBI Bookshelf

Dosing Lantus® (insulin glargine injection) 100 Units/mL
Insulin – Pharmacology, Therapeutic Regimens, and Principles of Intensive Insulin Therapy - Endotext - NCBI Bookshelf

Patient-Led Versus Physician-Led Titration of Insulin Glargine in Patients with Uncontrolled Type 2 Diabetes: A Randomized Multinational Atlas Study1 - Endocrine Practice

Lantus vs Levemir | Lantus® (insulin glargine injection) 100 Units/mL

Lantus Solostar (long acting basal Insulin Glargine)

Effects of Dulaglutide and Insulin Glargine on Estimated Glomerular Filtration Rate in a Real-world Setting - Clinical Therapeutics

Basal Insulin: Types, Benefits, Dosage, and Side Effects
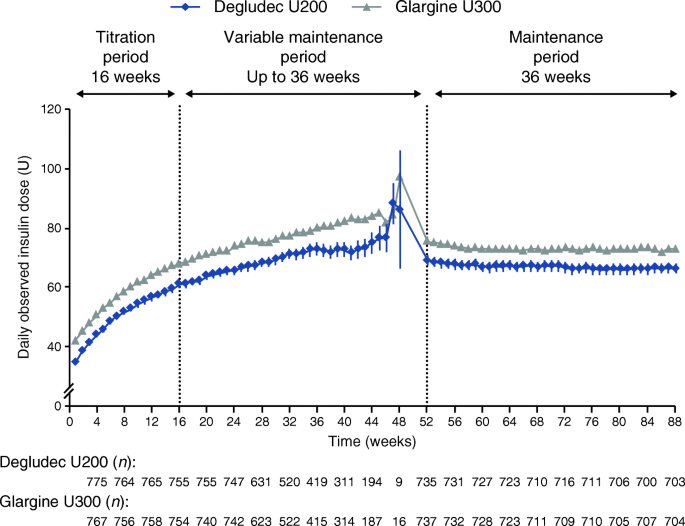
Risk of hypoglycaemia with insulin degludec versus insulin glargine U300 in insulin-treated patients with type 2 diabetes: the randomised, head-to-head CONCLUDE trial | SpringerLink

Improved Glycemic Control vs NPH | Lantus® (insulin glargine injection) 100 Units/mL

Long Acting Insulin - an overview | ScienceDirect Topics

Efficacy and safety of oral basal insulin versus subcutaneous insulin glargine in type 2 diabetes: a randomised, double-blind, phase 2 trial - The Lancet Diabetes & Endocrinology

Insulin – Pharmacology, Therapeutic Regimens, and Principles of Intensive Insulin Therapy - Endotext - NCBI Bookshelf
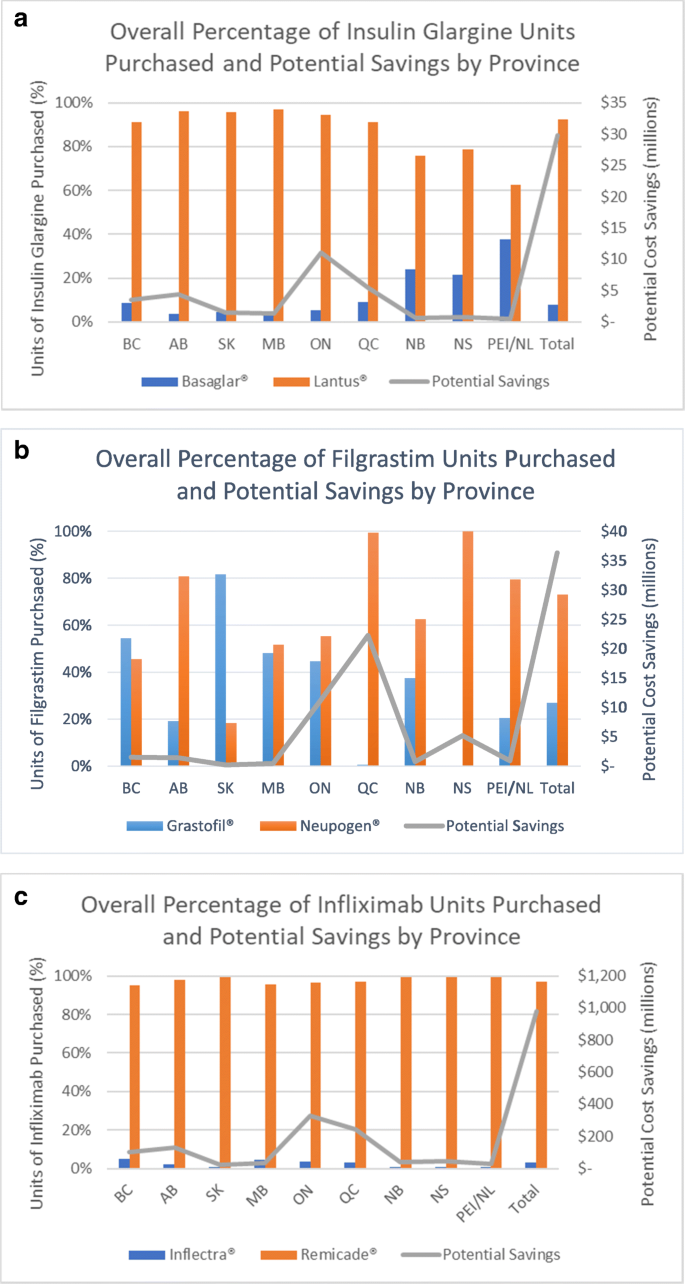
Correction to: Potential cost-savings from the use of the biosimilars filgrastim, infliximab and insulin glargine in Canada: a retrospective analysis | BMC Health Services Research | Full Text

Exenatide twice-daily does not affect renal function or albuminuria compared to titrated insulin glargine in patients with type 2 diabetes mellitus: A post-hoc analysis of a 52-week randomised trial - Diabetes Research

Insulin Management of Type 2 Diabetes Mellitus - American Family Physician

Mixing Insulin Glargine With Rapid-Acting Insulin: A Review of the Literature | Diabetes Spectrum
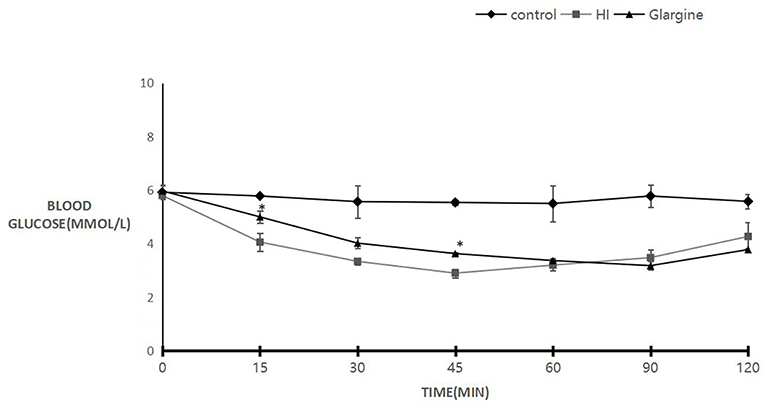
Frontiers | The Role of Insulin Glargine and Human Insulin in the Regulation of Thyroid Proliferation Through Mitogenic Signaling | Endocrinology

Insulin glargine: Side Effects, Dosage, Uses, and More

Durability of insulin degludec plus liraglutide versus insulin glargine U100 as initial injectable therapy in type 2 diabetes (DUAL VIII): a multicentre, open-label, phase 3b, randomised controlled trial - The Lancet Diabetes

Lantus 100 units/ml solution for injection in a cartridge - Summary of Product Characteristics (SmPC) - (emc)
Quality Department Guidelines for Clinical Care Inpatient

Glycaemic responses in Asian and non-Asian people with type 2 diabetes initiating insulin glargine 100 units/mL: A patient-level pooled analysis of 16 randomised controlled trials - Diabetes Research and Clinical Practice
Managing Dawn Phenomenon with Basal Insulin | Diabetes Strong
Posting Komentar untuk "which statement is correct regarding glargine insulin?"